A Squib by Dr Daniela Andrade, associate professor at Universidade do Vale do Rio dos Sinos
[bg_collapse view=”button-red” color=”#ffffff” icon=”arrow” expand_text=”What’s a Squib?” collapse_text=”Hide this explanation” ]
In the EM/CA community, we all know the importance of “putting our work out there”: discussing our findings and impressions with other researchers is not only a way to avoid (or at least reduce) the risks of an individualistic analysis, but also, and above all, a precious resource for progressing and improving our work. Long before the publication in a journal, in the midst of the analytic process, collective scrutiny and discussions are fundamental practices to provide the researcher with suggestions, comments, references and even beneficial doubts.
For this reason, this section of the ISCA Forum Newsletter is dedicated to “squibs”: concise articles containing preliminary, in-process analyses in an EM/CA perspective. In this section, researchers can present their work-in-progress findings to the ISCA community in order to generate discussions and collect observations, suggestions, useful references and potential publication venues.
CALL FOR CONTRIBUTIONS
Would you like to share your in-process analysis to have some feedback? Send us your squib! Please note that your contribution should satisfy the following requirements: 1) not exceed 2000 words (2200 for non-English data); 2) contain one or two transcripts and relative preliminary analyses; 3) illustrate a phenomenon fitting within the existing framework of EM/CA analyses.
Please email your contribution to pubs@conversationanalysis.org
[/bg_collapse]
CA-based research (e.g., Bergen et al., 2017, Koenig, 2011, Stivers, 2006, Street et al., 2005) has demonstrated how patients use the interactional machinery to resist healthcare providers’ recommendations (i.e., deontic actions, determining how the world should be, Stevanovic, 2011). Those might comprise medication, lifestyle, or health conditions monitoring. A recent study (Ostermann, in progress) shows that patients’ reluctance to accept healthcare-providers’ recommendations resides in a continuum between passive resistance and outright rejections. However, research on patient acceptance and resistance in this context has mostly concentrated on verbal actions – including the absence of verbal responses. Patients’ embodied responses to healthcare-providers recommendations received much less attention. Adopting a multimodal interactional approach that seeks to scrutinize visible conducts (Hepburn, Bolden, 2017) in this context may illuminate how the “complex organization of multimodal Gestalts” (Mondada, 2014a) materializes on the unfolding sequences of interest. With this study, I am interested in unveiling patients` embodied frameworks of participation (Mondada, 2014) that play a role in the resistance configurations, mainly in the context of (possible) lifestyle recommendations. My current main focus relies on looking at how the resistance and disaffiliation emerge in an “enchronic” frame (Enfield; Sidnell, 2017) and how participants disclose embodied conducts in the course of building actions.
The context of the study is an educational program concerning good-health practices that a private hospital in the south of Brazil accomplishes with Artery Coronary Syndrome (ACS) and Congestive Heart Failure (CHF) patients. The program consists of talks regarding lifestyle habits, and self-care conducts pursuing treatment adherence. For identity preservation, I renamed the educational program Maxcardio. The stated aim of Maxcardio is to reduce hospitalization rates.
The data consist of approximately 7 hours of video and audio recorded interactions involving a multi-professional team of healthcare-providers – physicians, nurses, nutritionists, physiotherapists, and psychologists – responsible for patients’ good health practice recommendation-delivery. Such healthcare-providers approach patients while they are in the hospital. The visits are not previously announced. Verbal and embodied conduct transcriptions followed Jefferson’s (1984) and Mondada’s (2019) conventions. The analysis of the dataset presented below is exploratory.
The segment of interest is part of a conversation between a heart-ill male patient and a female psychologist. The patient in Excerpt 1 has ACS and got hospitalized due to a heart attack. Furthermore, he presents morbid obesity, which leverages the risk factor to aggravate his heart conditions. To manage the right stakes of further heart complications due to the patient’s obesity, his cardiologist forwarded him for the bariatric surgery evaluation process. Although his medical records include several hospitalizations, this is his first time in the current hospital.
To approach heart-ill patients, the psychologist self-created a scripted talk. She introduces herself as the Maxcardio team member and explains how the Maxcardio program works (data not shown). We join the interaction amid her scripted multi-unit turn (notice the and-prefaced TCU) in which the topic revolves around the patient’s routine. The psychologist states the reason for the visit, namely, “to check his routine outside” [the hospital] (l. 2). She proposes that something in the patient’s daily routine caused this last hospitalization (l. 4-6), to which the patient agrees (l.7).
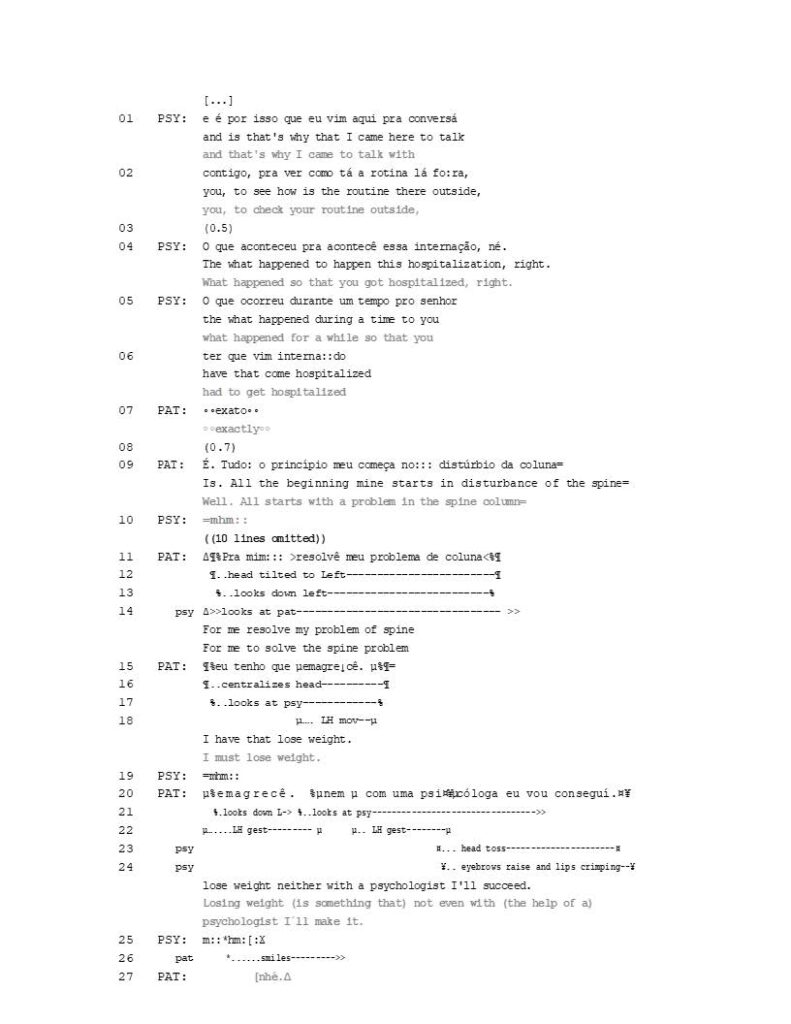
Excerpt 1 [HMD_PSY_MPAT_ACS_MO_7_24_13]
After a 0.7 gap (l. 9), the patient self-selects and initiates his turn with a delay token (“É”), which projects talk expansion. The expansion comes in the format of a trouble report-telling-preface TCU (Mandelbaum, 2013) (“Tudo: o princípio meu começa” – All starts) that indicates a course of action in the lines of trouble recounting (Jefferson, 1973). The trouble report telling (TRT) involves a spine column problem that caused him to become sedentary and, as a consequence, overweight (data not shown). Interestingly, nothing in the psychologist’s talk suggests that her visit concerns the matter of weight or the bariatric procedure. At this point, it is worth restating that the patient went to the hospital due to a heart problem in the first place and is in the cardiac ward. The patient himself selects to talk about weight gain as the topic regarding the possible “routine alterations’’ that might have caused him to get hospitalized.
The transcript restarts when the patient’s talk forwards to conclude the TRT sequence. He produces a multi-unit turn through which he manages to link the weight problem with the psychologist’s visit. This patient’s multi-unit turn is of particular interest for the analysis.
In lines 11-15, the patient launches the first TCU of the turn in which he elaborates what is supposedly the resolution of his spinal issue, i.e., losing weight. A combination of multimodal aspects in the trajectory of the TCU deserves inspection. First, the intonation contour of the TCU – the extended elongation of the word “mim” (me) together with thepitch fall in the last syllable of the word “emagrecê” (lose weight) – constitutes a prospective prosodic device for projecting turn-holding (Selting, 1995; Auer, 1996). Second, when he launches the TCU, his head is slightly tilted to the left, and his gaze is accompanying the head inclination, that is, left down directed. As the first TCU approaches possible completion (l. 15), specifically, the part in which he refers to his responsibility regarding resolving the spinal condition (“I must lose weight”), he centralizes his head and looks at the psychologist. At this point, he sustains his gaze towards her, suggesting an orientation to a competing activity (Rossano, 2013) (e.g., turn-taking). As he articulates the word “emagrecê” (to lose weight), he spins his left hand, half-twisting it and changing the palm position from down to up. After producing the word “emagrecê,” the patient receives a go-ahead (Schegloff, 2007); a continuer with “a low level of speakership incipiency” (Gardner, 2001: 5) (l. 19).
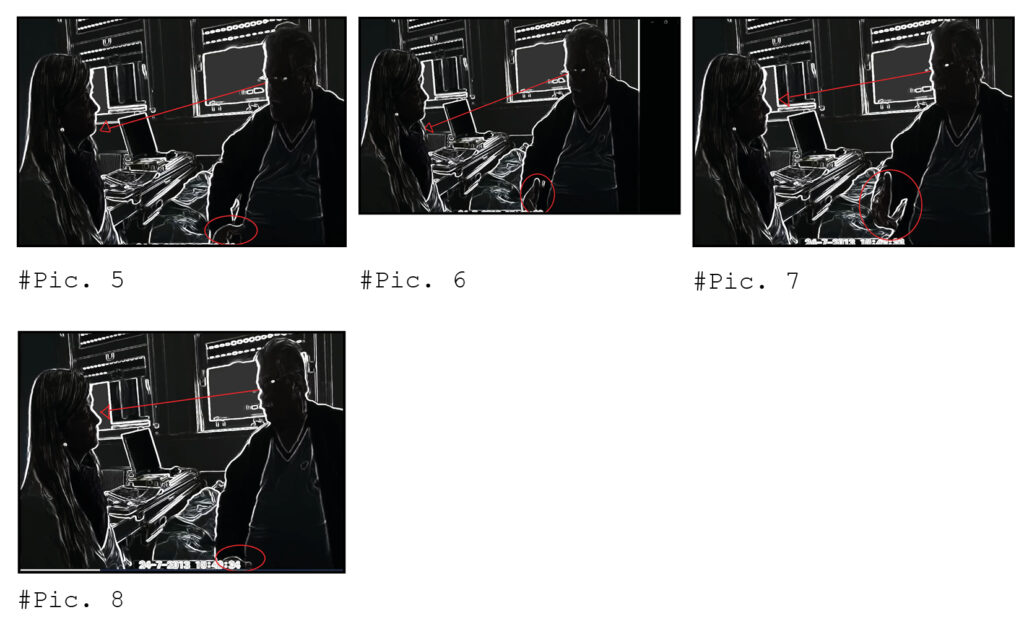
After the go-ahead, the patient begins to elaborate on the final part of his turn. Through this last turn’s TCU, the patient works to empty any possible intended project of making him lose weight through psychological aids (line 20). The patient finely constructs the anticipated resistance in multimodal ways that combine turn design, gaze, and hand gestures.
In terms of turn design, first, it is noticeable that the patient front-loads the nominated problem solution (losing weight), which suggests the topic as salient in the action formation (Levinson, 2013). The repetition of the word “emagrecê” (to lose wait) (l. 20) projects it as a disjunctive move from its most recent past use (Drew, 2013). Second, the patient selects inverted negative grammar (l. 20) when coherently connecting the TRT and the supposed resolution of his spinal problem to what he displays to understand from the psychologist’s motive for the visit. And third, he articulates the negative word embodied markedly through his third left- hand gesture.
Considering gaze, the patient shifts its direction as he launches the final part of his turn. At the beginning of this particular TCU, he averts his gaze from the psychologist to immediately redirect it towards her again as he starts to deliver the final part of the turn, namely, the part in which he evaluates psychological assistance as useless (to help him lose weight). He also coordinates talk and gaze shift together with two hand hits in the air. The hand gesture coordination with talk is especially interesting because the patient escalates their strength. The gesture salience increases as the core content of the talk changes from the out declared ‘best solution’ for the spinal problem to the presumed psychologist’s visit’s ineffectiveness.
Summarily, the patient repeats the hand movement three times. The first two times at the exact moment when he pronounces the word “emagrecê” (to lose weight), in lines 15 and 20, this last time in the front-load position. And the third time, as he pronounces “nem” (not even), again in line 20. The strength of the movements increases each time and reaches its peak in its third repetition; not coincidentally, in coordination with talk through which resistance outbreaks (Stivers, 2006), that is, together with the production of “nem” (not even), which, as previously argued, is articulated prominently. The escalation of the strength of the movement is represented in film clips 1 and 2. Film clip 1 shows the patient’s embodied behavior coordinated with talk transcribed in line 15. Film clip 2 demonstrates the patient’s embodied conduct coordinated with talk produced in line 20.
Film clip 1:

Film clip 2:
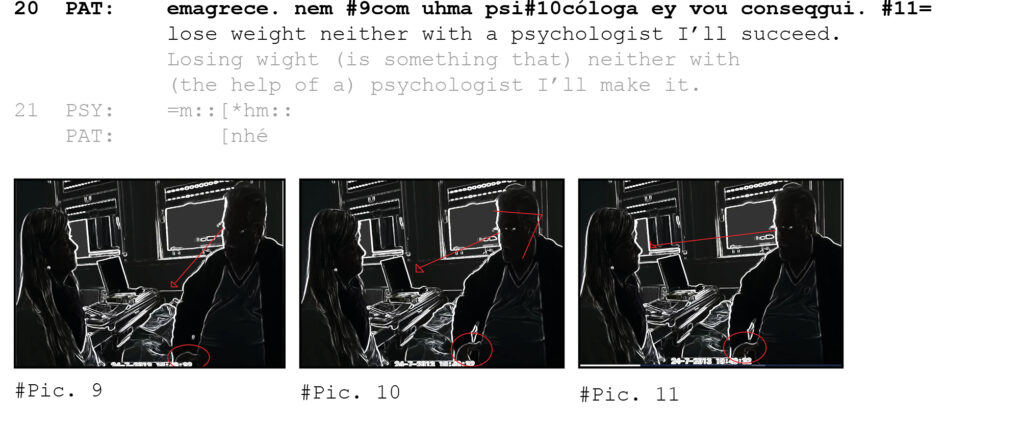
As the patient’s turn reaches completion, the psychologist responds with a long-stretching token (line 25), compared to the tokens produced by her in lines 10 and 19, which worked as continuers. The production of this last token happens when the psychologist has to deal with the highly social dispreferred manifestation of resistance against any approach she might have considered to the patient. Its salient articulation marks the psychologist’s stance as disaffiliative.
However, the psychologist’s disaffiliative stance appears consequential from the patient’s resistance much earlier than the long-stretching token production. It comes up precisely in line 20, as the patient produces the word “psychologist” stressed syllable (same as in English). As shown in the transcription, in lines 23-24, the psychologist starts to toss her head and raise her eyebrows while the patient is articulating the referred word. Film clip 3 aims to show the synchronicity between the patient’s resistance action and the psychologist’s response to it as it unfolds.
Film clip 3:
The disaffiliative stance of the psychologist does not go undetected by the patient, who responds with a post-completion particle (Clift, 2017), more specifically, a stand-alone “né” (Ostermann; Almeida, 2017), produced with laughter. The sequential location and design (Drew, 2013) of the patient’s turn that carries the stand-alone “né” intertwined with laughter suggest the patient is orienting to the potentially dispreferred character of evaluating psychological aid useless.
Resisting healthcare professionals’ recommendations may be interactionally laborious, but ‘‘patients regularly demonstrate the ability to influence events in their social worlds according to their preferences, needs, and desires’’ (Koenig, 2011: 1106). Patients may engender such influence by avoiding a course of action from occurring through anticipated resistance to the very undesired not-yet offered recommendation. The simple presence of an unrequired professional and an open question as the psychologist asked in this interaction may trigger an anticipated resistance.
The scrutiny of the patient’s embodied behavior in coordination with talk allows us to observe how he interactionally labors to resist in advance any possible lifestyle recommendation from the psychologist. The very fact that he delays the point at which resistance comes up to the surface explicitly demonstrates that he struggles to deliver it. The delay in delivering in conjunction with the choice of grammar and the strength of the hand gestures reveal the patient’s interactional achievement of resistance in intricate details.
The embodied layer added to the analysis “disclos[es] subtle socio‐interactional dynamics” (Mondada, 2016: 344). It shows the patient’s action configuration of resistance and also the psychologist’s early orientation to it in a disaffiliative way. Thus, it helped to investigate how the participants used resources and designs to construct social actions and relationships (Cruz; Andreatto, 2020).
I think investigating how resistance and disaffiliation emerge in the context recommendations through multimodal lenses may interest the CA community, mainly those involved in healthcare interactions. The next step of the study is to explore other excerpts in which the mobilization of multimodal resources helps to escalate resistance in lifestyle recommendations of different nature (smoke cessation and physical exercise).
If you have any comments, suggestions, and critics, I would be happy to hear to improve my work.
References
Auer, P. (1996) On the prosody and syntax of turn-taking in English. In Couper_Kuhlen, E. & Selting, M. (eds.). Prosody in conversation. Cambridge: Cambridge University Press, pp. 1-10.
Bergen, C., Stivers, T., Barnes, R., Heritage, J., McCabe, R., Thompson, L. & Toerien, M. (2018) Closing the Deal: A Cross-Cultural Comparison of Treatment Resistance, Health Communication, 33:11, pp. 1377-1388, DOI: 10.1080/10410236.2017.1350917
Clift, R. (2017) Conversation analysis. Cambridge: Cambridge University Press.
Cruz, F. & Andreatto, N. (2020) Um estudo exploratório da notação de gestos em interações com crianças altistas. Linguística e Semiótica, 24:47, pp. 81-102.
Drew, P. (2013) Turn design. In J. Sidnell, & T. Stivers (eds.), The handbook of conversation analysis.. Chichester: Wiley-Blackwell, pp. 131-149.
Enfield, N & Sidnell, J. (2017). The concept of action. Cambridge: Cambridge University Press.
Gardner, Rod. (2001) When listeners talk: response tokens and listener stance. Amsterdam: John Benjamins Publishing Company.
Hepburn, A. & Bolden, G. (2017). Transcribing for social research. Los Angeles: Sage Publications Ltda.
Jefferson, G. (1973) A case of precision timing in ordinary conversation: overlapped tag-positioned address terms in closing sequences. Semiotica, 9:1, pp. 47-96.
Jefferson, G. (1984). Transcript notation. In: J.M. Atkinson, & J. Heritage (Eds.), Structures of social action: studies in conversation analysis. (pp. ix-xvi). New York: Cambridge University Press, pp. ix-xvi.
Koenig, C. (2011) Patient resistance as agency in treatment decisions, Social Science and Medicine, 72: 7, pp. 1105–14.
Levinson, S. (2013) Action formation and ascription. In J. Sidnell, & T. Stivers (Eds.), The handbook of conversation analysis. Chichester: Wiley-Blackwell, pp. 103-130.
Manddelbaum, J. (2013) Storytelling in conversation. In J. Sidnell, & T. Stivers (Eds.), The handbook of conversation analysis. Chichester: Wiley-Blackwell, pp. 492-508.
Mondada, L. (2019) Conventions for multimodal transcriptions. Version, 5.0.1. <https://www.lorenzamondada.net/multimodal-transcription.>
Mondada, L. (2016) Challenges of multimodality: language and the body in social interaction. Journal of Sociolinguistics, 20:2, pp. 2-32.
Mondada, L. (2014a) The local constitution of multimodal resources for social interaction. Journal of Pragmatics, 65, pp. 137-156.
Mondada, L. (2014). Bodies in action: multimodal analysis of walking and talking. Language and Dialogue, 4:3, pp. 357–403.
Ostermann, A. (submitted). Women’s (limited) agency over their sexual bodies: Contesting contraceptive recommendations in Brazil.
Ostermann, A; Teixeira, C. (2017). Small things that matter a lot: The deontic nature of “né” in Brazilian Portuguese. Paper presented at the 8th World Congress of Applied Linguistics (AILA 2017), Rio de Janeiro, Brazil, July 23-27.
Rossano, F. (2013). Gaze in conversation. In J. Sidnell, & T. Stivers (Eds.), The handbook of conversation analysis. Chichester: Wiley-Blackwell, pp. 308-329.
Schegloff, E. (2007) Sequence Organization in Interaction: A primer in conversation analysis. 1 ed. Cambridge: Cambridge University Press.
Stevanovic, M. (2011) Participants’ deontic rights and action formation: The case of declarative requests for action. Interaction and Linguistic Structures (InLiSt), 52.
Stivers, T. (2006) Treatment decisions: negotiations between doctors and parents in acute care encounters. In Heritage, J. & Maynard, D. (eds) Communication in Medical Care: Interaction between Primary Care Physicians and Patients. Cambridge: Cambridge University Press.
Streeck, J., Goodwin, C., & LeBaron, C. (2011) Embodied interaction: language and body in the material world. New York: Cambridge University Press.
